Last week, the U.S. administration under the guidance of RFK Jr., released their updated version of the food pyramid.
It should come as no surprise that nearly everyone in my side of the world had something to say about it.
There were a handful of areas that did catch my attention, and, as I made a point to say on a social media post of mine, I think there are some positives, and some questionable parts to it.
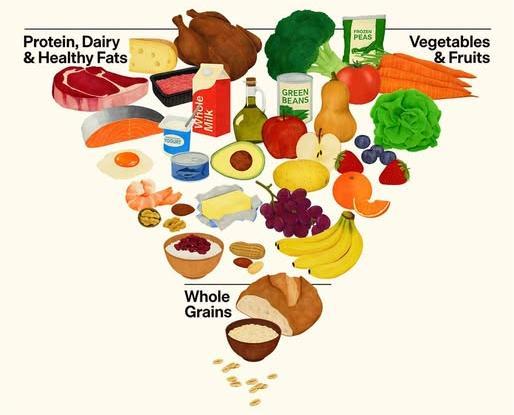
I should mention that there is the graphic of the pyramid (referenced below), a 10 page document giving more insight, and an additional 90 page document giving even further details.
While the graphic itself gives a snapshot of the direction the government is suggesting we go, it doesn’t tell the whole story.
So, let me dive into some areas I found of interest upon review.
Saturated Fats
I was admittedly concerned about this section prior to the release of the guidelines. Historically, I’ve been taught throughout numerous certifications I’ve completed based in both North America and the U.K., that our diets should be made up primarily of polyunsaturated and monounsaturated fats and that saturated fat should only comprise 10% of total fat intake. This information is based off of the association that increased saturated fat intake (dairy excluded) may also increase cardiometabolic risk.
There was the belief that there would be an emphasis on not demonizing saturated fat in the diets, and even when you look at the pyramid, the animal proteins featured would all be high(er) in saturated fat. It’s mentioned that saturated fat should take up no more than 10% of total caloric intake.
Here are some numbers to compare against: On my guidance, if your total calories from fat equate to 700 calories a day, that means that saturated fat only covers 70 of those calories. If you take the guidance of HHS, and your total caloric intake for the day is 2000, then 200 calories would be saturated fat.
I’ll say this, and it’s only my opinion, if heart issues run in your family, you may want to be more conservative with saturated fat intake.
Also, bear in mind that fat is 9 calories per gram. Fat has more calories per gram than any other macronutrient. If you’re someone who struggles to find a calorie deficit for fat loss, adding more fat into the diet will very likely work against you. This may explain why many people who go keto, low carb, and sometimes carnivore, tend to find themselves back at maintenance or a surplus of calories because they overshot their fat intake (and calories by default.)
Protein
I believe the HHS got this part mostly right. Prior to this release, most of the guidance from the government about protein intake kept you from being malnourished and those numbers were admittedly quite low.
Now, there’s a range that I feel far more comfortable with: 1.2-1.6g of protein per kg of bodyweight. So, a 200lb person would aim for 110-145g of protein per day. Just a reminder that you don’t have to be perfect, but you may want to stay close in that range and it’s okay if you overshoot it a bit (assuming you don’t have a medical condition suggesting otherwise.)
Also, if you’re using a GLP-1 receptor agonist medication to help with fat loss, protein requirements go a long way (coupled with strength training) to help you maintain muscle mass.
My only knock on the protein suggestions, is that there is very little visual emphasis on the graphic to consider the needs of vegans and vegetarians. The documents give better guidance in that department. Also, many women struggle with whey (dairy) based protein powders and may need to choose plant based options for better digestive outcomes.
Whole Grains
To be honest, I was disappointed in this part. In the graphic, whole grains represent the smallest part of the pyramid. In a world where carbohydrates are routinely demonized, grains appear to take the hit in the visual. They get slightly more grace in the documents. I know and appreciate that everyone’s digestive systems are different and many people do not tolerate grains.
For me, they are a necessity. I can eat as many fibrous vegetables and fruits as my heart desires but if I don’t get some fibrous grains in there, the plumbing won’t work right.
As for you, you do need to understand what works best for your body but bear in mind that grains have existed successfully in other cultures for eons and they’re not demonizing them.
I do appreciate that many grains have been fortified with extra ingredients and some people snub their noses when they see what they believe to be too many ingredients on a food label and assume that it makes something unhealthy. I say: the “poison” is in the dose. Anything can be consumed to unhealthy amounts (even water) so you do need to be aware of your personal thresholds. Also, there needs to be recognition that for people who struggle with poverty and/or live in food deserts, fortified grains may be the very best they can do for themselves.
Alcohol
This one is murky for me. We now have substantial evidence that no amount of alcohol is healthy. It is even suggested that more and more people are turning to sobriety as drinking rates appear to be dropping: A 2025 Gallup poll found only 54% of U.S. adults drink, the lowest in nearly 90 years, down from 67% in 2022.
However, the HHS is being more conservative about it, only saying that people should “consume less alcohol for better
overall health.” Dr. Oz himself (not someone I would qualify as being an expert in nutrition), claimed it was a “social lubricant.”
I’m not going to stand in a glass house throwing stones. My wife and I both enjoy a nice (measured) serving of bourbon. We don’t drink to get drunk, it’s a complement to a meal. We both understand the relative risk and, like a lot of things, you’ll need to proceed as you see fit.
What I will say, is that if the optimization of health is your primary aim, then no alcohol would be the path.
Additional Thoughts
While it would be impossible to cover every exception to health guidelines in 10-90 pages of documentation, I do feel there are certain demographics that wouldn’t be well-served by the pyramid.
Individuals struggling with IBS and IBD may benefit from a tailored, individualized, low FODMAP approach to eating. Many “healthy”, “real” foods can be problematic for these people and can exacerbate their symptoms. I’ve written several times about this approach on my site if you need some guidance there.
Also, there is little consideration for people who struggle with disordered eating behaviors. When our government chooses to look at foods as “good” vs “bad”, this can also play into an all-or-nothing mindset for those with eating disorders. What’s healthy and appropriate for one, may not be the same for another, but demonizing foods is typically a problematic way to foster a healthy relationship with our bodies and the food we eat.
I know it’s “en vogue” to speak poorly of processed foods (or more specifically, highly-processed foods), but they aren’t problematic for everyone. Taking a cue from above, sometimes, it’s all that some people can afford. While I would much rather someone grab some whole fruits over some Doritos, we should have enough mental flexibility, that if you want to eat a chip, then eat the damn chip.
If you’ve determined that chips are not a food you can easily moderate, then credit should be given to improving the food environment (what you have direct access to in the home.)
For people who have certain dietary intolerances, (I’ll use gluten as an example), their options for gluten free alternatives are often highly processed. That doesn’t inherently make them less healthy. Everyone deserves to find a food substitute that allows them to cook recipes they will enjoy when a food is otherwise offensive to their bodies.
One last thing, I’m not convinced that many people put their lives into food pyramids, no matter which government rolled them out. People don’t necessarily need a visual graphic telling them what to eat when behavior modifications drive so many of our food decisions.
A quote I found on the internet, credited to RD Dr. Kevin Klatt, “If you want to know why most dietitians push back on the “eat real food” framing, it’s because most of us have worked in clinical practice, seen people literally starving to death from disease, & had the patient or a well-meaning family member question enteral feeding because formula isn’t ‘real food’.”
Perhaps the next version of the food pyramid will have some evidence based guidance on how to improve our food environment, coping skills when we struggle with emotional eating, and perhaps an advisory board that isn’t abundantly low carb in nature and ideology.
Leave a comment